Since your jawbone is covered with skin and soft tissue, you can’t see what is happening under the surface. So, when you start having issues with bone loss in jaw areas, it’s possible that this condition might go undetected.
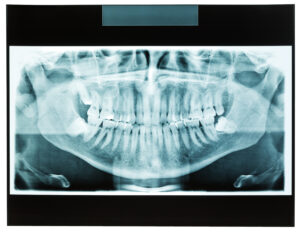
The most important thing that you can do is maintain regular dental checkups because our experienced team uses modern digital imaging to see what is happening deep within your mouth. We can look at the structure of your jaw, teeth, and gums with the goal of identifying potential issues in the earliest stages.
Bone Loss in the Jaw: Why it Happens
The jawbone is a strong foundation to support the teeth and protect your facial structure. While the bone often maintains its shape and density for healthy patients, there are various factors that can increase the risk of this jawbone deterioration.
Why would the jaw bone start to deteriorate? Several lifestyle and health factors can impact the jawbone, causes a deterioration of bone density over time:
- Untreated Gum Disease: Chronic inflammation and infection in the gums takes a toll on jaw bone health. The bacteria from the infection destroys the soft tissue and supporting bone, which leads to a decrease in bone density. This is one of the reasons why it’s critical to seek treatment for periodontitis as soon as possible.
- Missing Teeth: If you are missing teeth, then it can increase the risk of jawbone loss. The jawbone requires constant stimulation from the chewing motions that happen naturally throughout the day. But when the tooth is missing, then the root of the tooth is no longer stimulating the jawbone. As a result, it can lead to severe bone loss.
- Osteoporosis and Other Conditions: Not only does osteoporosis cause jaw bone density loss, but it can also weaken the rest of the bones throughout the body. If you have been diagnosed with osteoporosis, then it’s important to consult with your general physician as well as an experienced dentist to minimize the complications from this condition. Other health conditions can also increase the risk of bone density loss.
- Poorly Fitted Restorations: If you are wearing dentures or bridges that don’t fit your mouth properly, then it can increase the risk of your jawbone deteriorating. These appliances put pressure on the gums and jaw, which accelerates bone loss.
- Smoking and Lack of Nutrition: Patients who smoke or use tobacco have a much higher risk of bone density loss because the chemicals from smoking reduce blood flow in the gums. Additionally, it’s essential to maintain a healthy diet because deficiencies of calcium and Vitamin D can cause your bones to weaken.
The people who are most at risk are patients with missing teeth, chronic gum disease, wearing dentures long-term, and smokers. Additionally, diabetic patients have a higher risk of bone loss in the jaw due to chronic inflammation and the way circulation is affected.
Bone Loss in Jaw: Symptoms to Watch For
Some of the most common symptoms of jawbone deterioration include:
- Loose Teeth & Receding Gums: When the gums start to recede, it’s usually an indication of gum disease. This chronic infection causes the gums to deteriorate, and also affects the strength of the teeth. You might notice that your teeth are shifting or loosening. If these symptoms are happening, then it is likely that your jawbone is also being affected.
- Tooth Sensitivity: Pay attention if you notice that one or more of your teeth have become more sensitive unexpectedly. Gum recession can cause the roots to be exposed, which increases the risk of sensitivity. It’s likely that you are losing jawbone mass as well.
- Tooth Extraction: If you need to have one or more teeth removed, then there is an increased risk of bone loss in that area. Since the tooth roots are no longer in the jaw, the empty space can start to deteriorate. This is one of the reasons why dental implants are often recommended after extraction, because the implant post helps to preserve the jawbone.
- Facial Changes: When bone volume decreases, it means that you don’t have as much support to maintain facial structure. So, patients with severe jaw bone loss start to develop an aged or sunken look.
- Difficulty Speaking or Chewing: As jaw bone loss progresses, normal daily activities can become more challenging. For example, you might have problems chewing or speaking.
Early Detection: Identifying Bone Loss in Jaw Before It’s Too Late
As with many other dental issues, the key to reducing the risk of major complications is to take a proactive approach with early detection. The sooner you diagnose that you are losing bone mass in jaw, the better the long-term outcome.
At-home monitoring and oral health habits are helpful, but nothing compares to having a consultation with an experienced dental team. If you suspect that you are having any dental issues, including gum disease, toothache, and/or bone loss, then it’s time to consult with our dental team.
We use digital dental x-rays as a way to assess your bone health and see if there are any warning signs of bone deterioration. By using these imaging tools during regular checkups, we can catch the issues before you develop more severe symptoms.
Additionally, there are times when it makes sense to use more advanced imaging solutions, such as 3D cone beam scans. This type of imaging gives us a more detailed view of your jawbone density. We can identify structural changes that are happening, then recommend treatment options to help.
Is It Possible to Stop or Reverse Bone Loss Jaw Issues?
Modern dentistry offers multiple options to promote healthy jawbone density. If our dental team diagnoses any issues relating to bone loss, then we might recommend specific treatments to support the overall density and strength of your jaw bone.
- Bone Grafts: Sometimes, bone grafts can be used to rebuild lost bone. This treatment is often paired with the placement of dental implants for patients who are missing teeth.
- Dental Implants: Not only does a dental implant replace the tooth that you are missing, but the placement of the post in the jawbone is beneficial for preserving jawbone density.
- Guided Tissue Regeneration (GTR): Another modern dental treatment can encourage natural bone growth as needed. This method is a safe and effective solution to consider.
- Oral Health and Prevention: Don’t underestimate the importance of maintaining good brushing and flossing habits each day. When you are staying consistent with these oral health habits, it can have a positive impact on preventing gum disease and bone loss. If you have already been diagnosed with gum disease or bone loss, then these daily habits might slow the progression.
FAQ:
How fast does jaw bone loss occur?
After a tooth is extracted, it is possible for bone loss to start within six months. Jaw bone loss will progressively continue without dental interventions.
How do I know if I have bone loss in my mouth?
Watch for the common symptoms listed above, including difficulty chewing, receding gums, loose teeth, and changes in your facial structure.
What are the first signs of osteonecrosis of the jaw?
Some of the most common symptoms of osteonecrosis include jaw pain, exposed bone, swelling, and slow healing after you have dental procedures. If you notice these symptoms, then you should talk to your dentist right away for treatment recommendations.
How to reverse bone loss in jaw?
Bone loss can be reversed using bone grafts, dental implants, and proper oral health habits. Our dental team can offer recommendations for bone regeneration.
How much bone loss before teeth fall out?
If you lose 30 – 50% of the bone around a tooth, then it causes instability that could cause the tooth to fall out.
Talk to the Dental Experts
For more information about available services, explore our restorative dentistry options. At myDental, we offer family-friendly services and a range of treatments. Schedule an appointment at one of our convenient locations.